“Code Blue!” Picture these scenarios:
- After receiving the change-of-shift handoff, you enter your patient’s room to introduce yourself and do a quick assessment. The patient has been stable since their uncomplicated surgical procedure, but now they aren’t breathing.
- The wife of another nurse’s assigned patient comes running down the hall and grabs you, yelling, “My husband just ‘fainted’ and I can’t wake him up!” You follow her to the patient’s room and find the man unconscious in his bed, without a pulse.
- An elderly woman is visiting her son who is recovering from a kidney transplant. The son puts on his call light. When you respond, he screams that his mother suddenly collapsed and fell on the floor. You quickly determine that she isn’t breathing.
You have your Basic Life Support (BLS) certification. What will you do NOW?
What is a Code Blue or RRT?
“Code Blue” is when a patient experiences an unexpected cardiac or respiratory arrest, requiring immediate resuscitation and activation of a hospital-wide alert. The alert includes a location, such as a floor and room number or a department.
When you’re the first one who discovers someone (besides a patient, it could also be a visitor or another staff member) who is not breathing or who has no pulse, YOU are the one responsible for initiating Code Blue., whether or not the person is your assigned patient.
NOTE: Many acute care settings also have “Rapid Response Teams,” or RRT, comprised of a physician, ICU nurse, respiratory therapist, and other staff, such as a nursing supervisor, pharmacist, or X-ray technician. The RRT is called when a patient’s condition deteriorates rapidly, their vital signs are unstable, or they are in acute distress. The patient isn’t coding yet, but they likely will progress to code status without immediate interventions.
What do you do FIRST after you call Code Blue?
- Take a nanosecond to calm yourself. Focus on the task at hand. You’ve got this!
- You are the First Responder. Call for help AND start CPR. If there’s a Code Button in the room, hit that, too.
- Quickly note the time you encounter the person and begin CPR.
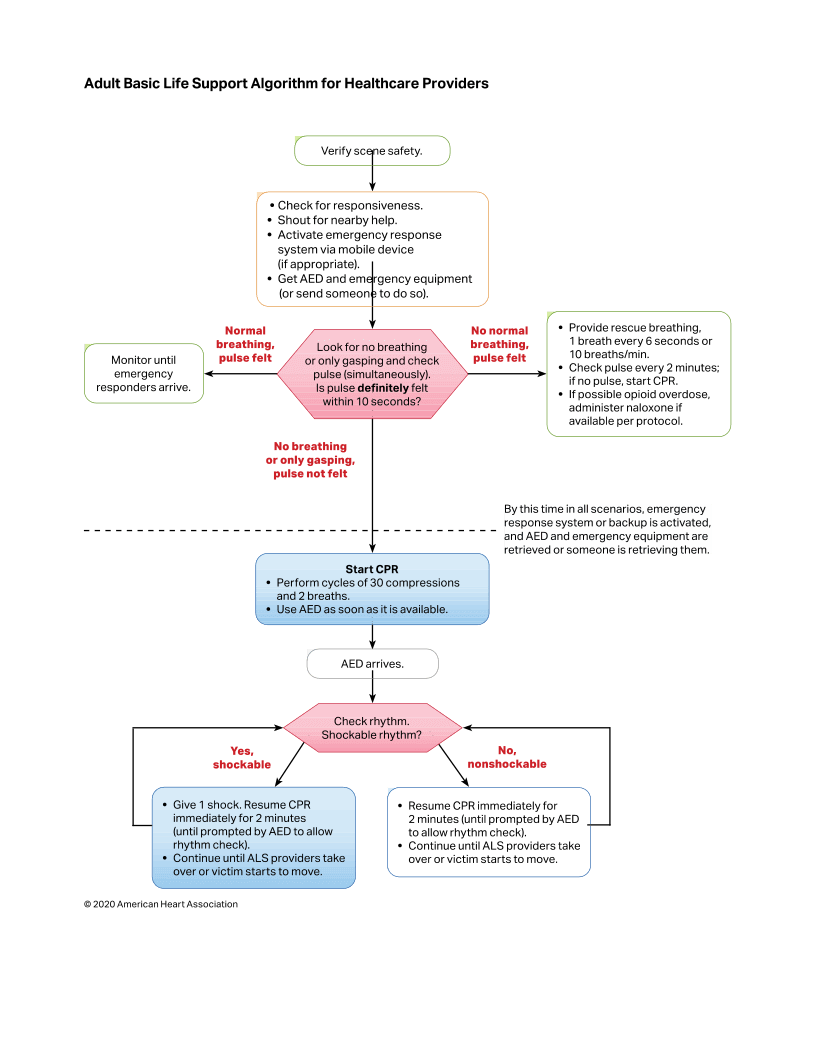
- Another nurse or respiratory therapist—Second Responder--should get an AMBU bag and hook it up to 100% oxygen (Turn the O2 all the way up) and start bagging the patient). The current (2000) American Heart Association Adult BLS Algorithm calls for cycles of 30 compressions and 2 breaths.
- A third nurse should quickly get the Crash Cart and AED and bring them to the location. Continue with CPR until the Code Blue or RRT arrives. When the team arrives and the Code Team Leader takes over, you’ll be directed to step back.
- Communication is key! Every Code Team member announces their role when they enter the room. There may be a lot of people, but everyone has a responsibility. It’s an example of “controlled chaos.”
What’s your role as the Primary RN?
- Remember that the Code Team or RRT know nothing about this patient! YOU are the best source of information.
If the patient is assigned to you, be prepared to provide essential information to the Code Team:
- What happened immediately prior to the code
- Recent vital signs
- Lung sounds
- Admitting diagnosis
- Surgery and procedures this admission, if relevant
Be accurate and concise about the patient:
- Age/Race/Gender
- Recent test and lab results
- Medical history related to the situation/admission
- Last breathing treatment, if administered
- If you think you know what the problem is, SAY IT!
Be prepared to assist. You may be asked to:
- Administer IV medications
- Hang fluid boluses
- Get an ECG
- Administer antibiotics
- Titrate O2
- Check on a bed in ICU
- Announce what you’re doing when ordered by the Code Leader. “Hanging a 250 mL bolus.” “Getting an ECG.” “Bed available in ICU.” (Closed-loop communication, see next step)
- If you’re able to be a bystander, pay close attention to the roles of the Code Blue team members, especially the Code Leader. AHA guidelines requires that all communication during a code be “closed-loop” with the leader. For example, the leader may “open the loop” by ordering “Push 1 mg of epinephrine now.” The team member responsible for drugs will administer it and state, “1 mg of epinephrine administered.” This “closes the loop” for that specific order.
What are common roles of Code Blue team members?
Role | Responsibilities |
Code Leader | Directs all roles, provides orders in “closed-loop” communication, assesses the patient, decides if/when the code continues or is “called.” |
Primary/Medication RN | Provides patient information, in charge of the patient’s IV access sites, administers medications provided by the Code cart controller. (If there is no specific medication nurse, the patient’s primary nurse assumes this role.) |
Crash Cart controller | Oversees the Crash Cart: Breaks the lock and opens the cart, organizes and distributes the items as directed, including medications. Announces each medication being prepared and distributed to the Medication RN. |
Chest compressor(s) | Performs high-quality chest compressions. Notifies team leader when relief is needed, so another team member can take over. The First Responder performs this role until the Code Team arrives. |
Airway manager | Opens and secures the patient’s airway, oversees supplemental O2 administration, monitors pulse oximeter, sets up and manages suction, assists respiratory therapist or anesthesiologist. |
Defibrillator manager | Applies defibrillator pads, follows orders to analyze rhythm and shock, clears team from the patient prior to administrating shocks. |
Documenter / Timekeeper | Tracks time of all interventions and announces intervals to the team leader. Documents all interventions on the required ACLS flowsheet. |
Runner | Retrieves supplies and medications. And completes actions (such as procuring PPE or calling for an ICU bed) outside the code area. |
Crowd controller | Excludes nonessential staff and people from the code setting, assists in transport of patient’s roommate, provides support for the patient’s family members if they are present and/or observing. |
Cleanup crew | Cleans the room after the code. Sweep and pick up sharps, discarded drug ampules and supplies. Assist primary nurse with postmortem care, if applicable. |
Adapted from American Journal of Nursing, A. Anderson, July 2019, Vol. 119, No. 7
American Heart Association Adult BLS Algorithm for Healthcare Providers
What can you do after the code?
- First of all, recognize that there is no such thing as a perfect code. Tension is high, communication may be abrupt and confusing, and team members may not be familiar with each other. There may be delays in receiving lab or X-ray results. The patient’s condition may contribute to uncertainty about how to proceed with the resuscitation.
- Take a few minutes to calm yourself. Reflect on everything you did and saw. Remembering that no code is perfect, what can you learn from this one?
- Is there something that you still need to learn?
- Is there anything you could do differently next time?
- Did you observe anything a code team member did that you would improve on if you had the chance?
- Is there a role that you could see yourself doing in the future?
- Would it be useful to take the ACLS course?
- Codes can stir up strong emotions. If the Code Blue team has debriefing meetings, try to attend if you were an observer. Besides reviewing the code, sometimes the team gets to talk about their feelings around the situation. Otherwise, talk to your preceptor, an experienced nurse, or the unit manager about the code and how you felt.
- If possible, examine the Crash Cart before it gets returned. Notice where the medication drawer is (it gets removed and placed on top of the cart) and what medications are included. Check out the airway and intubation supplies. You’ll be more comfortable in future codes if you know what items will likely be used. Handle the defibrillator to see how it feels.
- Don’t get tripped up on “What if…?” (“What if I’d checked him sooner?” “What if I wasn’t sure she’d stopped breathing?”) Maybe you feel guilty because you didn’t anticipate the patient’s sudden decline or you wish you’d recognized their increasing distress. Every nurse wants to keep their patients safe and avoid a crisis. You did your best, but sometimes circumstances are out of your control.
- Finally, reframe the situation. Return to the facts of the code and its outcome. Everything possible was done according to current evidence-based medicine and guidelines. If the patient was resuscitated and moved to ICU, everyone on the Code Team—including you--was successful. Well done! If the code was called after all ACLS protocols were attempted but the patient died, look at the root cause. Perhaps it was the patient’s diagnosis, a complication of surgery, or a physiological reason that was undetected.
- Even though you will gain knowledge and confidence with each code, you’ll also learn that every code is different. Do your best and know that you are making every effort to help your patient survive and return to health.
 By
By 



